The venous drainage of the gallbladder is unusual since the fundus and the body drain directly into the liver via the gallbladder fossa, which in turn drain into the intrahepatic portal radicals of segment V and IV of Couinard – the two segments between which the gallbladder lies. There is also direct drainage of the venules in the gallbladder fossa into the sinusoid, creating another unique portal circulation. (Moore)
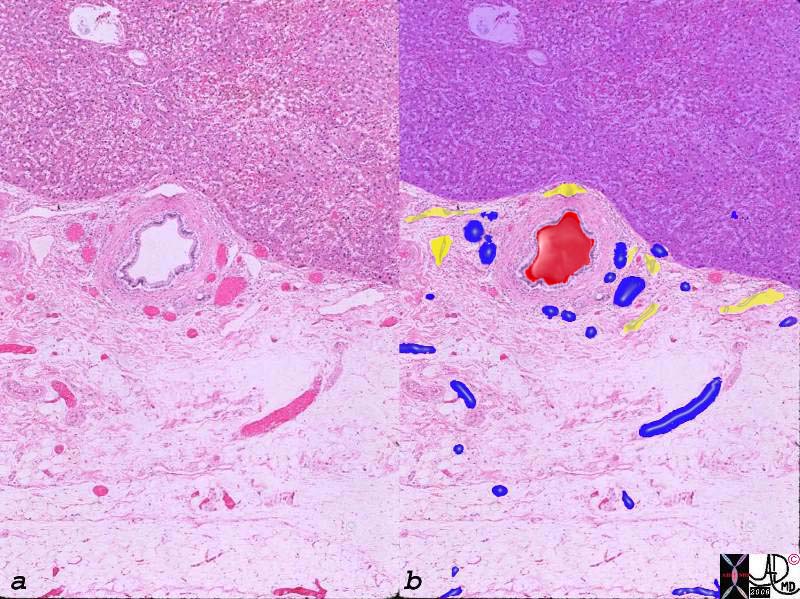
Arteries, Veins and Lymphatics in the Gallbladder Fossa |
|
The histological section of the gallbladder fossa shows the relatively large thick walled branch of the deep cystic artery, abutting the liver (upper portion purple) accompanied by venules (blue) and lymphatics. The veins drain directly into the fossa and connect with intrahepatic portal branches of the segment V and IV of the liver. 00140c03.8s gallbladder wall gallbladder fossa normal artery duct liver interface histopathology |
Venous drainage of the neck and cystic duct are drained by the posterior and anterior cystic veins which join with the gastric, duodenal, and pancreatic veins to empty into the right portal system.
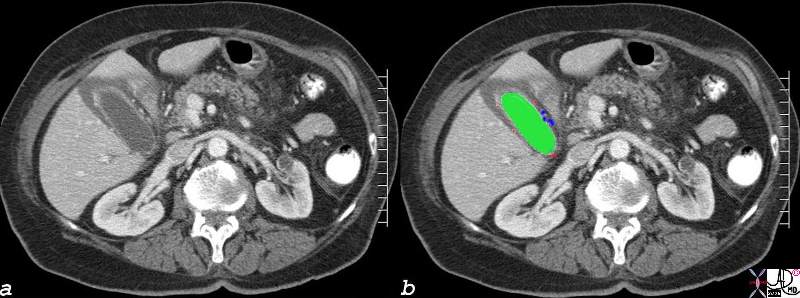
Cystic Arterioles and Venules in the Submucosa |
| The CTscan during portal venous phase shows a gallbladder with edematous wall, and contrast enhanced mucosa and small punctate vessels in the lamina propria. Some of these vessels are small and well defined and are presumably areterioles, (red) while others at the base of the gallbladder are slightly larger, (blue) suggesting that these may be venules draining the neck.
82006c05.8s liver gallbladder blood supply hepatic artery cystic artery cystic arterioles submucosa wall edema hyperemic mucosa red = hepatic artery green = lumen of the gallbladder CTscan Courtesy Ashley Davidoff MD Copyright 2008 |
The main final common pathway of gallbladder venous drainage is via the right portal vein which receives venous blood both from segments V and IV, and also directly from the cystic veins at the base of the gallbladder. Once the portal venous radicles perfuse the sinusoids blood reaches the middle or right hepatic veins before entering the inferior vena cava. (Yoshimitsu )
Applied Biology
Circulatory and inflammatory diseases result in venous and lymphatic congestion leading to an increase in extracellular fluid. In right heart failure for example the increased right sided pressures reflect in venous congestion of the liver and gallbladder edema can result. This is especially prominent in patients with right heart failure and with tricuspid regurgitation.
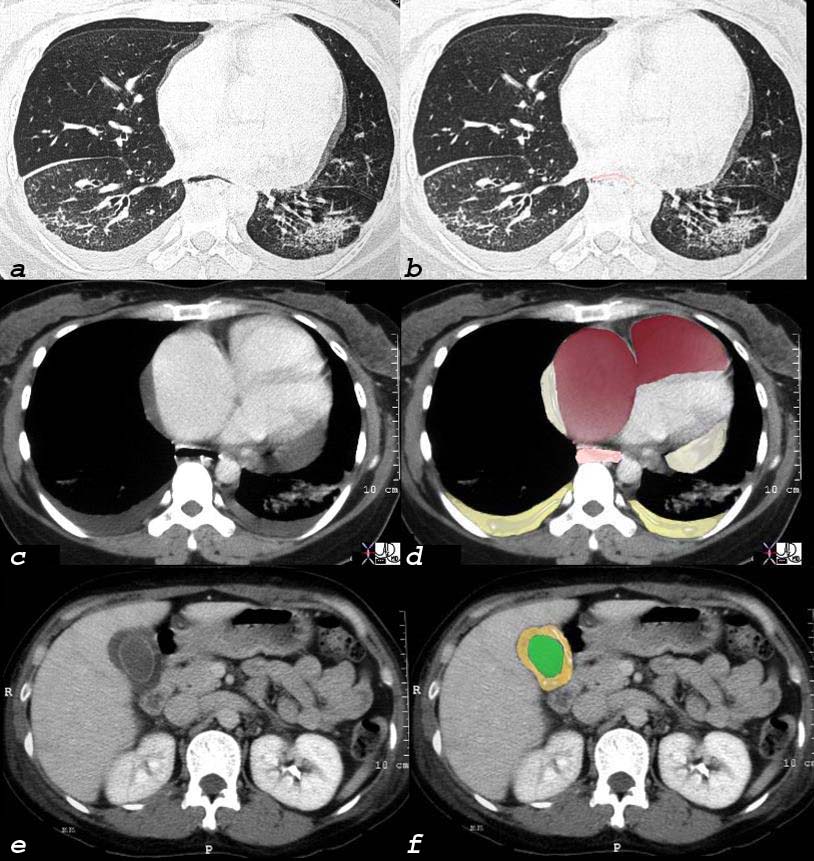
Scleroderma Pulmonary Hypertension and Right Heart Failure |
|
This 32 year old female has scleroderma and her disease is characterized by interstitial basal lung disease (a,b) with normal anterior lung fields and fibrotic posterior lung fields, enlargement of right heart structures (maroon in d), pericardial effusion (light yellow in d), pleural effusions (dark yellow in d) and an edematous wall (orange, in f) of the gallbladder (lumen is green). As a result of her lung disease she developed pulmonary hypertension, right heart failure and tricuspid regurgitation and this lead to the gallbladder edema. and 30464c08 32 female lungs pleura heart cardiac RA RV right ventricle right atrium pericardium gallbladder esophagus ILD basal interstitial lung disease pericardial effusion pleural effusion cardiomegaly enlarged esophagus patulous esophagus gallbladder wall edema congestive cardiac failure RHF right heart failure pulmonary hypertension cor pulmonale dx scleroderma CTscan Courtesy Ashley Davidoff MD |
Inflammation of the gallbladder and liver are also characterized by exudation of fluid due to hyperemia, and increased capillary leakage as a normal response by the body to the noxious agent. The increased extravascular fluid, may accumulate either by design to dilute the noxious agent or as a result decreased drainage of an overwhelmed lymphatic syatem that fails to drain effectively. As a result fluid may accumulate in the soft tissues of the gallbladder and the fluid is often visible to radiologic imaging.
Venous varicocities are formed as a result of portal hyperetension or portal vein occlusion with the development of new collaterals that encompass the gallbladder. Two examples follow
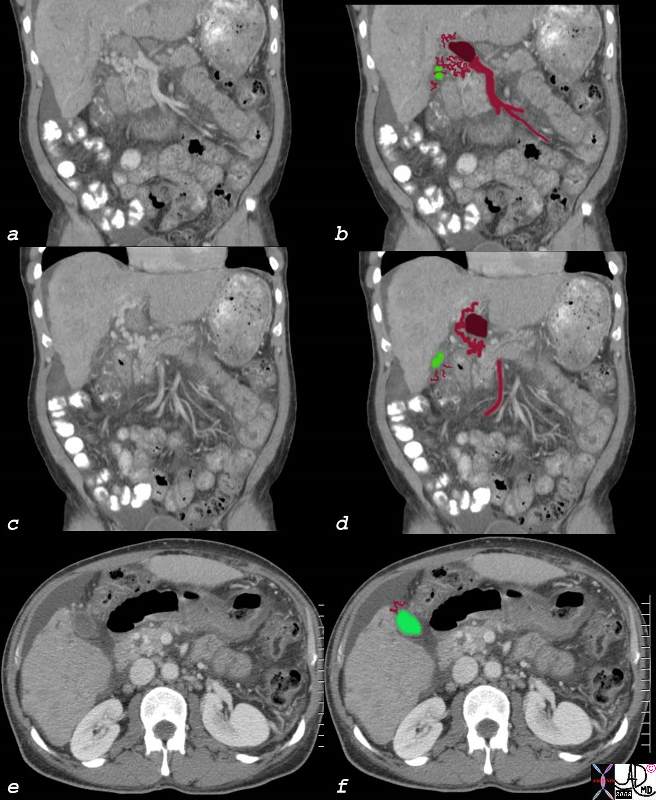
Gallbladder Varicosities |
| In the CTscan above the coronal images (a,b,c,d) show thrombus (maroon) in the portal vein causing obstruction and the development of serpiginous collaterals called cavernous transformation of the portal vein. Sometimes these varicocities involve the gallbladder (green) as seen in image e and f in cross section.
82709c01.8s 60M liver HCC hepatocellular carcinoma portal vein thrombosis hepatic vein thrombosis cavernous transformation of the portal vein gallbladder varicosity ascites CTscan Courtesy Ashley Davidoff MD copyright 2008 CTscan |
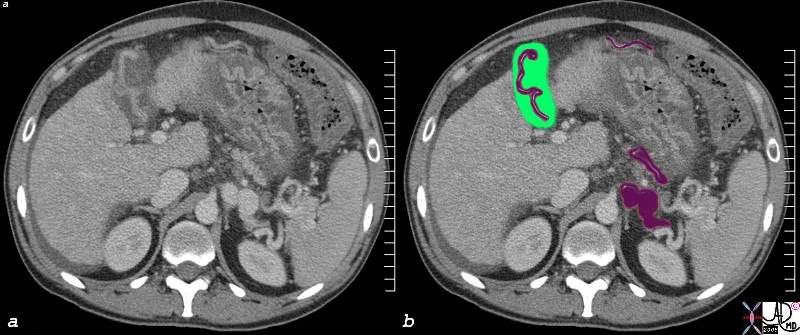
Gallbladder Varicosity |
| In this CT scan through the upper abdomen, portal hypertension has also manifest with patent venous varicosities (maroon) in the splenic hilum, over the gallbladder and with an enlarged gastroepiploic vein The stomach shows signs of a hypertensive gastropathy with thickened wall and hyperemic mucosa, there is a small amount of ascites behind the liver, and the caudate lobe is enlarged. These findings are consistent with cirrhosis and portal hypertension.
82117c.8s liver cirrhosis caudate lobe enlarged gallbladder varicose vein varicosity stomach wall thickened hyperemeic gastroesophageal varices ascites colon thick walled CTscan Courtesy Ashley DAvidoff MD copyright 2008 |
References
Ito Ket al Gallbladder disease: appearance of associated transient increased attenuation in the liver at biphasic, contrast-enhanced dynamic CT. Radiology. 1997 Sep;204(3):723-8.
Matsui O, et al. Staining in the liver surrounding gallbladder fossa on hepatic arteriography caused by increased cystic venous drainage. Gastrointest Radiol. 1987;12(4):307-12.
Sugita M, et al. Intrahepatic inflow areas of the drainage vein of the gallbladder: analysis by angio-CT. Intrahepatic inflow areas of the drainage vein of the gallbladder: analysis by angio-CT. Surgery. 2000 Sep;128(3):417-21.
Yoshimitsu et al Anatomy and Clinical Importance of Cholecystic Venous Drainage: Helical CT Observations During Injection of Contrast Medium into the Cholecystic Artery AJR 1997:169:505-510
